Abstract
Background
High-Intensity Interval Training (HIIT) involves bursts of high-intensity exercise interspersed with lower-intensity exercise recovery. HIIT may benefit cardiometabolic health in people with nonalcoholic steatohepatitis (NASH).
Aims
We aimed to examine the safety, feasibility, and efficacy of 12-weeks of supervised HIIT compared with a sham-exercise control (CON) for improving aerobic fitness and peripheral insulin sensitivity in biopsy-proven NASH.
Methods
Participants based in the community [(n = 14, 56 ± 10 years, BMI 39.2 ± 6.7 kg/m2, 64% male), NAFLD Activity Score 5 (range 3–7)] were randomized to 12-weeks of supervised HIIT (n = 8, 4 × 4 min at 85–95% maximal heart rate, interspersed with 3 min active recovery; 3 days/week) or CON (n = 6, stretching; 3 days/week). Safety (adverse events) and feasibility determined as ≥ 70% program completion and ≥ 70% global adherence (including session attendance, interval intensity adherence, and duration adherence) were assessed. Changes in cardiorespiratory fitness (V̇O2peak), exercise capacity (time-on-test) and peripheral insulin sensitivity (euglycemic hyperinsulinemic clamp) were assessed. Data were analysed using ANCOVA with baseline value as the covariate.
Results
There were no HIIT-related adverse events and HIIT was globally feasible [program completion 75%, global adherence 100% (including adherence to session 95.4 ± 7.3%, interval intensity 95.3 ± 6.0% and duration 96.8 ± 2.4%)]. A large between-group effect was observed for exercise capacity [mean difference 134.2 s (95% CI 19.8, 248.6 s), ƞ2 0.44, p = 0.03], improving in HIIT (106.2 ± 97.5 s) but not CON (− 33.4 ± 43.3 s), and for peripheral insulin sensitivity [mean difference 3.4 mg/KgLegFFM/min (95% CI 0.9,6.8 mg/KgLegFFM/min), ƞ2 0.32, p = 0.046], improving in HIIT (1.0 ± 0.8 mg/KgLegFFM/min) but not CON (− 3.1 ± 1.2 mg/KgLegFFM/min).
Conclusions
HIIT is safe, feasible and efficacious for improving exercise capacity and peripheral insulin sensitivity in people with NASH.
Clinical Trial Registration Number
Australian New Zealand Clinical Trial Registry (anzctr.org.au) identifier ACTRN12616000305426 (09/03/2016).
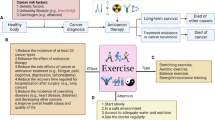
Graphical Abstract

Similar content being viewed by others
Introduction
Nonalcoholic steatohepatitis (NASH) affects up to 30% of people with NAFLD and is characterized by liver necroinflammation, severe insulin resistance and cardiometabolic dysfunction. With disease progression largely driven by insulin resistance [1], NASH affects up to 37% of people with type 2 diabetes (T2DM) [2, 3]. NASH is strongly associated with cardiovascular disease morbidity and mortality and increases the risk of liver cirrhosis, hepatocellular carcinoma and a range of extrahepatic malignancies [4].
NASH management centers on lifestyle modification addressing diet quality and increasing physical activity aiming for ≥ 7–10% body mass reduction. However, this magnitude of weight loss is difficult to achieve and harder to sustain [5]. Regular aerobic exercise can effectively reduce liver fat, irrespective of weight loss [6]; however, there is a dearth of literature examining the utility of exercise in people with NASH. Since 2003, there have been data reported on a total of ~ 50 exercising participants with confirmed NASH across six studies [7,8,9,10,11]. Cross sectional evidence has demonstrated an inverse relationship between vigorous physical activity and NAFLD severity [12]; however, these observations rely on self-report data, which are limited by recall bias and cannot inform treatment effects in established NASH.
High-intensity interval training (HIIT) involves bouts of high-intensity exercise interspersed with passive or active recovery periods. Emerging longitudinal evidence from small clinical trials have suggested that HIIT elicits comparable reductions in liver fat to traditional moderate-intensity continuous training [13]; however, these studies have not included people with biopsy-confirmed NASH. HIIT is a potent exercise modality for improving aerobic fitness [14]. This is relevant since low cardiorespiratory fitness is associated with higher NAFLD prevalence and increased risk of death in people with NAFLD [15]. In clinical and laboratory-based settings, HIIT appears to be safe and effective for cardiometabolic health improvement in people with chronic disease, including T2DM and cardiovascular disease, when conducted with adequate screening, testing and monitoring protocols [14, 16, 17]. HIIT may therefore be an effective modality for improving cardiometabolic and liver health in people with NASH.
Importantly, for a therapeutic option to be broadly translated into clinical care options, the target prescription needs to be feasible, i.e., the prescription (including target intensity) needs to be both safe and achievable. People with NASH commonly report chronic fatigue, poor sleep, musculoskeletal issues, impaired physical functioning, reduced capacity for activities of daily living and low engagement with physical activity [18,19,20,21], which might impact the ability to exercise. The pathophysiology of NAFLD is also associated with exercise intolerance and diastolic and autonomic dysfunction [22,23,24]. In addition to traditional barriers to physical activity, namely time, exercise-related knowledge, and access to facilities, these condition-centered factors may affect the capacity and desire to do vigorous physical activity. Therefore, the objectives of this study were to examine the safety, feasibility, and efficacy of 12-weeks of supervised HIIT for improving aerobic fitness and metabolic health in people with biopsy-confirmed NASH.
Patients and Methods
Trial Design
The study was a randomized controlled trial, registered prospectively with the Australian New Zealand Clinical Trial Registry (ACTRN12616000305426). All research was conducted in accordance with both the Declarations of Helsinki and Istanbul. Ethical approval was granted by the Metro South and University of Queensland Human Research Ethics Committees. Participants provided written informed consent prior to participation in the study. The study is reported in line with CONSORT and Consensus on Exercise Reporting Template guidelines.
Participants
Participants were recruited between June 2016 and February 2020 from a specialist hepatology outpatient unit within a local hospital and health service. Inclusion criteria were: (i) aged 18–70, (ii) not meeting general physical activity guidelines (< 150 min of moderate or < 75 min of vigorous aerobic exercise per week or relative combination of both), (iii) NASH confirmed by liver biopsy and (iv) ability to read, write, and speak in English. Exclusion criteria included significant contraindications to exercise testing/training, or any other reason which would limit the ability to participate in the study (Supplementary Material 1: Methods).
Randomization: The randomization sequence (1:1 ratio) was generated by a researcher outside of the investigator team using pre-generated lists of permuted blocks (www.randomization.com). Following the completion of baseline assessments, participants were given a sealed opaque envelope containing group allocation (by SK). Participants were randomized into either: (i) control (CON) or ii) exercise intervention (EX). Participants randomized to CON were invited to undertake the 12-week supervised HIIT intervention after completing their 12-week control period, with repeat outcomes assessed at week 24 (Fig. 1).
All assessments were undertaken at the School of Human Movement and Nutrition Sciences at The University of Queensland (UQ), except for magnetic resonance imaging and spectroscopy (Centre of Advanced Imaging, UQ) and the euglycemic hyperinsulinemic clamp (Clinical Research Facility, Princess Alexandra Hospital, Brisbane, Australia). No study assessments or intervention/control visits were conducted between March to November 2020 due to COVID-19-related restrictions. This resulted in the withdrawal of one participant who had undertaken all baseline assessments and randomization but had not commenced supervised HIIT and impacted the ability to recruit to target of 22 participants.
Intervention
Exercise Intervention (EX)
Participants in EX completed three sessions of HIIT per week for 12-weeks supervised by a qualified exercise professional. Because of the known high prevalence of musculoskeletal issues in people with NASH, a suite of exercise modalities was available to emulate real-world clinical practice and enhance the translatability of the approach for ongoing trials. The preferred mode was treadmill running/walking with gradient; however, stationary cycling, rowing ergometry and arm ergometry were available for those with musculoskeletal limitations. Sessions commenced with a 5-min warm-up at 60% of maximal heart rate (HRmax) followed by 4 × 4 min intervals at 85–95% HRmax interspersed with 3-min ‘recovery’ periods at ~ 60% HRmax, then a 5 min cool-down. For appropriate progression, in Week 1 participants were required to achieve at least 1 × 4-min interval, in Week 2 at least 2 × 4-min intervals, in Week 3 at least 3 × 4-min intervals and in Week 4 at least 4 × 4-min intervals so that in Weeks 5–12, all participants were completing the full 4 × 4-min protocol each session. Participants were instructed to commence intervals at a rating of perceived effort (RPE) of 15/20 on the Borg scale (license #5RYHYG) [25] and to achieve their target heart rate by the final minute of interval one and by the final two minutes of intervals 2–4. Heart rates were recorded by the exercise professional using a heart rate monitor (Polar, Polar Electro, Kempele, Finland) at the end of each minute and RPE within the final 15 s of each minute. Blood pressure was monitored using the auscultation method during interval and recovery periods to ensure blood pressure during exercise remained within specified safe limits [26]. Verbal encouragement was provided by the exercise professional during the high-intensity intervals. Absolute work rates were progressed during the 12-week training period to maintain relative exercise intensity (verified by heart rates and RPE).
Control (CON)
Participants randomized to CON undertook a 12-week supervised stretching program (30 min, 3 days per week, estimated energy expenditure negligible) described as a ‘pre-conditioning program’ prior to the HIIT intervention for the purpose of ‘blinding’ participants to the control condition (i.e., participants were unaware that they were randomized to the ‘control’ arm, with allocation labelled ‘stretch + HIIT’). This was designed to control for factors such as attention and participation without cardiometabolic effect.
Outcomes
Primary Outcomes
Safety was determined by number of HIIT-related serious adverse events (SAE) and adverse events (AE) reported during the study period (Supplementary Material 1: Methods). Participants were questioned about SAE and AE occurrence at the beginning of each exercise or control session, and relation to the study (as determined by the study physician).
Feasibility (Adherence to HIIT) was assessed by ‘program completion’ as well as session, intensity and duration adherence, which was used to calculate global adherence using our published guideline [27].
Program Completion was determined as feasible if ≥ 70% of participants who started HIIT, completed the 12-week program.
Session Adherence was determined as feasible if ≥ 70% of sessions were attended (from a possible 36 sessions).
Intensity Adherence number of intervals from Weeks 5–12 where the heart rate and/or the RPE criteria were met. Intensity adherence was determined as feasible if ≥ 70% of intensity targets were met.
Duration Adherence number of intervals completed per session from Weeks 5–12. Duration adherence was determined as feasible if ≥ 70% of intervals (out of four) were completed.
Global Adherence number of participants that met the feasibility criteria for all adherence variables. Overall, the supervised HIIT intervention was determined feasible if ≥ 70% of participants met the criteria for global adherence.
Adherence to CON number of sessions attended from the possible 36.
Secondary Outcomes
All assessment (except for the exercise test, detailed in Supplementary Material 1: Methods) were conducted after an overnight fast (≥ 10 h), and 24 h abstaining from exercise, caffeine, or alcohol. Post-assessments were completed between 24 and 72 h after the last bout of exercise. The individuals who conducted the assessments (e.g., healthcare practitioners and technical assistants) were blinded to participant group allocation, except for anthropometric measurements, which were undertaken by a primary researcher (SK). Prior to assessment visits, participants were instructed to not reveal their group assignment.
Aerobic fitness was assessed as cardiorespiratory fitness and exercise capacity.
Cardiorespiratory fitness (V̇O2peak) was determined via a symptom limited maximal cardiopulmonary exercise test (CPET) using a ramp exercise protocol under medical supervison. Participants were instructed to avoid exercise for 48 h, caffeine and tobacco for 24 h and food in the 2 h prior to the test. Treadmill was the preferred mode although a cycle ergometer was available for participants with musculoskeletal limitations that precluded walking/jogging to maximal capacity. The same test modality was used across assessment time points. Heart rate was recorded at rest and at the end of each minute, RPE and blood pressure every 2–3 min, and a 12-lead ECG was continuously monitored by a physician. A technical assistant blinded to group allocation provided the verbal encouragement to attain maximal effort. Pulmonary gas exchange (Parvo Medics TrueOne, Sandy, Utah, USA) was measured for 3 min prior to the start of the graded exercise test and then for the test duration. V̇O2, carbon dioxide production (V̇CO2) and minute ventilation (V̇E) were sampled using ten-second rolling averages.
Treadmill protocol Participants commenced walking at 4 km/hr and 0% grade for 2 min, followed by 4 km/hr and 4% grade for 2 min. Speed was then increased by 1 km/hr every 3 min and grade by 1% every minute until volitional fatigue or other test termination criteria [26].
Cycle protocol After a 4 min warm-up at RPE 10–12 and 60 revolutions per minute, work-rate was increased by 25 W per minute until volitional fatigue or other test termination criteria [26].
Cardiorespiratory fitness (V̇O2peak) was determined as the average of the two highest 10 s averages that were within plateau criteria (i.e., ≤ 150 mL/kg difference). The Ventilatory threshold (VT) and the V̇E/V̇CO2 slope were also determined using data from the exercising component of the CPET, excluding the first minute of exercise to remove the influence of hyperventilation. VT was determined manually as first sustained rise in the V̇E/V̇O2 without a simultaneous rise in the V̇E/V̇CO2 and was verified by two technicians. The V̇E/V̇CO2 slope was determined using the formula V̇E(L.min-1) = m(V̇CO2, L.min-1) + b, where m = V̇E/V̇CO2 slope and b = constant.
Exercise capacity was determined as time-on-test to the nearest second, calculated in seconds from the start of the warm-up to the cessation of the test.
Peripheral insulin sensitivity was evaluated by a 2-h euglycemic hyperinsulinemic clamp technique (3 h for those with diabetes) with a protocol mirroring that of Croci and colleagues [24] and supervised by an endocrinologist. Teflon catheters were placed into an antecubital vein for infusions, and into a heated dorsal hand vein to achieve arterialisation of venous blood, for sampling. Insulin (Humulin R;Eli Lilly, Indianapolis, IN) was prepared as a primed continuous infusion (40 mU/m2 body surface area/min) in 50 mL saline, at a rate of 15 mL/hr for clamp duration. Plasma glucose concentration was monitored every 5–10 min using an automated glucose analyzer (VerioIQ, Jounson & Johnson Medical Pty Ltd) [28], and a 25% glucose solution was infused at a variable rate, to reach steady state euglycemia. Blood samples were drawn at 20-min intervals. The mean value of the last four measurements of the steady state clamp period were used in all the analyses.
Total glucose disposal (TGD), a measure of peripheral insulin sensitivity, was calculated as the maximum glucose infusion rate at the end of the clamp. TGD was then normalised for fat-free mass, based on dual-energy x-ray absorptiometry (DXA)-derived fat-free mass (FFM) of the legs (i.e., KgLegFFM, see below).
Body composition and anthropometrics Body composition (total and regional fat percentage and lean mass) were quantified using DXA (Hologic QDR4500W Discovery, or Hologic Horizon A, Hologic Inc., Bedford, USA) and analysed using DXA software (APEX Version 4.5.3, Hologic Inc). Due to body size limitations, most participants had one or more arms outside of the field of view. Thus, android fat percentage was the principal body fat outcome and FFM was determined as right leg + left leg fat-free mass (KgLegFFM).
Waist circumference was measured against the skin to the nearest 0.1 cm using a metal retractable tape at the midpoint between the lowest rib and the iliac crest. All measures were taken in triplicate. Body weight was recorded to the nearest 0.1 kg and height to the nearest 0.1 mm.
Magnetic resonance imaging was used to quantify abdominal visceral (VAT) and subcutaneous adipose tissue (SAT), using previously reported methods [29]. SAT and VAT volume were quantified using commercial software (SliceOmatic version 5.0rev8d; Tomovision, Montreal, Canada).
Liver-related health Intrahepatic lipid was quantified using proton-magnetic resonance spectroscopy (1H-MRS) and analysed using software (jMRUI version 4.0, EU Project, http://www.jmrui.eu/) as previously described [29]. Liver biochemistry [alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (GGT)] were analysed by an accredited commercial laboratory.
Other metabolic health parameters Total cholesterol, HDL- and LDL-cholesterol, triglycerides, glucose, and insulin were measured after an overnight fast and analysed by an accredited laboratory. Systolic and diastolic blood pressures were taken in triplicate, in a darkened and thermoneutral room after 15-min quiet rest. The Metabolic Syndrome Severity Score was calculated [30] using R-software.
Health-related quality of life was assessed using the chronic-liver disease questionnaire [31].
Biochemistry Plasma Glutathione Peroxidase (GPx) Activity, High mobility group box 1 protein (HMGB1), Total Adiponectin, Intercellular Adhesion Molecule 1 (iCAM-1), High sensitivity C-reactive protein (HsCRP), and Cytokines [interleukin-6 (IL-6), interleukin-10 (IL-10) and tumor necrosis factor-alpha (TNFα)] were assessed after an overnight fast. Full methodology for biochemistry analyses is detailed in Supplementary Material 1: Methods, with all methods as per manufacturers’ instructions.
Vascular health Vascular function was measured via brachial artery flow-mediated dilation (FMD), in accordance with published guidelines [32]. Briefly, reactive hyperaemia was induced via arterial occlusion for 5 min using a sphygmomanometer cuff, with high-resolution ultrasound used to measure the change in brachial artery diameter and mid-artery pulsed Doppler signal for hyperaemic velocity. All recordings were analysed using specialised, automated, edge-detection and wall-tracking software, and were blinded for analysis. Assessment of haemodynamic indices and arterial stiffness were completed using a SphygmoCor® XCEL (AtCor Medical Pty Ltd., Sydney, Australia). For pulse wave analysis, a brachial cuff was placed around the brachial artery of the right arm, between the elbow and shoulder. Carotid-to-femoral pulse wave velocity (cfPWV) was used to assess arterial stiffness [33]. A cuff was placed around the mid-thigh and a tonometer pressure sensor on the carotid artery, to simultaneously capture the pulse waveforms at femoral and carotid sites. The velocity of pulse transfer from the carotid artery to the femoral artery was measured (using the direct method) and calculated according to standardised guidelines [34].
Habitual physical activity and habitual diet intake Participants were instructed not to alter their usual physical activity and dietary behaviours for the duration of the study period. Participants were provided with an accelerometer (GT3X + ; ActiGraph, Pensacola, FL or GeneActive; device consistent for pre-and post-intervention assessment for all participants) and asked to wear this on their nondominant wrist (Geneactive) or waist (ActiGraph) for 24 h for 7 days with raw acceleration data extracted and processed (Supplementary Material 1: Methods). Usual daily dietary intake was assessed at each time point by a diet history collected by a trained Dietitian and analysed using Foodworks (Xyris Australia).
Statistical Methods
Sample Size
This trial was powered to detect change in cardiorespiratory fitness and insulin resistance outcomes; however, COVID-19 interrupted the ability to recruit to target (n = 22) and so feasibility (safety, adherence) is presented as the primary outcome. However, with the sample size of 14 achieved, this offered adequate power to detect change in fitness based on the following assumptions: (i) baseline fitness level of ~ 22 mL/kg/min, (ii) a clinically meaningful ~ 15% improvement [35,36,37] with training, and (iii) a standard deviation of change in V̇O2peak of 1.5 mL/kg/min. These give a relative effect size of 2.09 compared with control. To detect this predicted minimum clinically meaningful difference, 10 participants (five in each arm) were required to achieve an actual power of 90% with 5% level of significance (G-Power software, University of Trier, Trier, Germany). Assuming a 30% loss to follow-up, a total of 13 participants were required.
Data Analysis
Data were analysed using SPSS version 27 (IBM, Armonk, New York, USA). Normality testing was performed using the Shapiro–Wilk test with visualisation of histograms and Q-Q plots of the residuals. A nonparametric test equivalent was used if the assumption of normality was still violated after data were transformed (natural logarithm). The primary analyses were between-group comparisons for EX vs CON examined via intention-to-treat analysis using ANCOVA with the difference (change score) as the dependant variable and the baseline value entered as a covariate. There was no imputation for missing data as this was deemed inappropriate based on the size of the sample. Effect sizes are reported as ƞ2 (eta-squared), which measures the proportion of variance associated with each main effect and interaction effect in an ANOVA model and is calculated as the between-group sum of squares/total sum of squares. These were interpreted as: small effect (0.01); small-to-medium effect (0.01–0.09); medium-to-large effect (0.10–0.25) and large effect (> 0.25) [38]. We further termed < 0.01 as negligible. A secondary analysis included the participants originally allocated to CON who then completed 12 weeks of the HIIT protocol. For this analysis, data was pooled from the HIIT periods for EX (baseline and Week 12) and CON (Week 12 and 24), and within-group changes were determined via paired t-tests or Wilcoxon test. Continuous variables are reported as mean ± SD, and categorical variables are reported as frequencies/percentages unless otherwise stated. Significance was set at p < 0.05. Authors SK, IH, JC, GAM designed the protocol and SK analysed data with biostatistcal support and can vouch for integrity of data analyses.
Results
Participant Flow and Recruitment
Fourteen eligible participants (nine men, five women) undertook the initial assessment and randomization (Fig. 2). Baseline characteristics are presented in Table 1. Most HIIT sessions were conducted individually with the maximum number of participants simultaneously training being two. All CON sessions were conducted individually. The mode of HIIT in those randomized to EX was treadmill (n = 6) and cycle ergometer (n = 1). In those randomized to CON who subsequently undertook the HIIT protocol, the mode was treadmill (n = 1), cycle ergometry (2), arm ergometry (n = 1) and rowing ergometry (n = 1).
Safety
No SAE or AE were reported relating to the study. There was one SAE reported in EX that was deemed to be unrelated to the study intervention (fall during daily living requiring hospitalisation). Three pre-existing musculoskeletal conditions (tendinopathies) required a continuation of their ‘usual care’ management in EX [stretching (n = 3) and isometric holds (n = 1)].
Feasibility
Adherence to HIIT Data regarding program completion and session, duration, intensity, and global adherence to supervised HIIT in the pooled sample (i.e., HIIT undertaken by both EX and CON) are shown in Table 2. All twelve participants commenced HIIT (n = 7 from EX and n = 5 from CON). There were three ‘drop-outs’ during HIIT within the first three weeks (n = 2 from EX and n = 1 from CON). The remaining nine participants (n = 5 from EX and n = 4 from CON) completed the full 12-weeks. All nine participants met the criteria for session adherence, duration adherence, and intensity adherence and therefore global adherence was 100% (Table 2). Collectively, when considering program completion and global adherence to the predetermined feasibility criteria, supervised HIIT was deemed feasible in people with NASH. Attendance to CON sessions was 90 ± 8.2%.
Secondary Outcomes
Table 3 contains outcomes data from between-group comparisons. Reasons for missing data for each outcome variable are listed in Supplementary Material 2: Table S2.
Aerobic Fitness
There was no between-group difference for change in cardiorespiratory fitness (V̇O2peak, EX -0.6 ± 2.0 mL/kg/min and CON 0.1 ± 0.1 mL/kg/min). There was a large between-group effect for exercise capacity, with time on the graded exercise test improving in EX (106.2 ± 97.5 s) but not CON (− 33.4 ± 43.3 s) (Fig. 3A). This included one drop-out in EX who returned to complete the CPET and reduced time-on-test by -21 s. For the secondary within-group analysis, pooling baseline and post-HIIT data for the ten participants who undertook HIIT (n = 6 in EX and n = 4 in CON), the mean improvement (95% CI) following HIIT was 106.2 s [(49.9 to 162.5 s); Fig. 3B)]. No between-group differences were observed for change in VT or the V̇E/V̇CO2 slope (Table 3).
Exercise Capacity (time-on-test, s). A Primary analysis EX (n = 6) vs CON (n = 5) for exercise capacity. Black solid lines = EX individual participant data; Black dashed line = EX group mean; Gray solid lines = CON individual participant data; Gray dashed line = CON group mean. Box-and-whiskers represent minimum, Q1, Q3 and maximum. *p value is for between-group change via ANCOVA; η2 = 0.44 (large effect). B Secondary analysis of pooled EX + CON HIIT training data (n = 10). Black solid line = individual pooled data; Black dashed line = group mean data; Box-and-whiskers represent minimum, Q1, Q3 and maximum. *p value is for within-group change via paired t-test
Peripheral Insulin Sensitivity
There was a large between-group effect for change in peripheral insulin sensitivity with EX improving by 1.0 ± 0.8 mg/KgLegFFM/min and CON reducing by 3.1 ± 1.2 mg/KgLegFFM/min (Table 3; Fig. 4A). For the secondary within-group analysis, when pooling baseline and post-HIIT data for the seven participants who undertook HIIT and could complete the clamp (n = 4 in EX and n = 3 in CON), the mean improvement following HIIT was 2.5 ± 3.0 mg/kgLegFFM/min (Fig. 4B). Moreover, in EX, one participant lowered their total daily basal insulin dose by 73% and another by 50%.
Peripheral Insulin Sensitivity (M, mg/kgLegFFM/min). A Primary analysis EX (n = 4) vs CON (n = 3) for insulin resistance. Black solid lines = EX individual participant data; Black dashed line = EX group mean; Gray solid lines = CON individual participant data; Gray dashed line = CON group mean. Box-and-whiskers represent minimum, Q1, Q3 and maximum. *p value is for between-group change via ANCOVA; η2 = 0.32 (large effect). B Secondary analysis of pooled EX + CON HIIT training data (n = 7). Black solid line = individual pooled data; Black dashed line = group mean data; Box-and-whiskers represent minimum, Q1, Q3 and maximum. *p value is for within-group change via paired t-test
Body Composition
There was a large between-group effect for change in BMI (− 0.9 ± 1.1 kg/m2 in EX vs 0.4 ± 1.4 kg/m2 in CON) and a medium-to-large between-group effect for change in waist circumference (− 3.5 ± 3.4 cm; -2.7% in EX vs 0.2 ± 3.3 cm; + 1.5% in CON) (Table 3).
A small-to-medium between-group effect was observed for android fat (− 1.6 ± 1.1% in EX vs 0.7 ± 1.3 in CON) with a small between-group effect for change in leg lean mass. There was a medium-to-large between-group effect for change in abdominal SAT (− 624.7 ± 199.6cm3 in EX vs 346.5 ± 636.5cm3 in CON, Table 3). A large between-group effect was observed for change in VAT (− 290.3 ± 815.2cm3 in EX vs 545.0 ± 617.3cm3 in CON) (Table 3).
Liver-Related Health
A large between-group effect was observed for change in intrahepatic lipid (− 6.0 ± 5.9% in EX vs -2.5 ± 9.9% in CON) with no meaningful change in liver enzymes (Table 3).
Other Metabolic Health
A large between-group effect was observed for change in total cholesterol (EX -0.6 ± 0.7 mmol/L vs CON 0.1 ± 0.3 mmol/L). There was also a medium-to-large between-group effect for the Metabolic Syndrome Severity Score with EX reducing by -0.2 ± 0.8 arbitrary units and CON increasing by 0.4 ± 0.6 arbitrary units (Table 3). There were small-to-medium between-group effects for changes in HDL-C, TG, fasting glucose, fasting insulin and DBP and a negligible between-group effect for change in SBP (Table 3). One participant in EX ceased antihypertensive medication during the HIIT intervention.
Health-Related Quality of Life
There was a large between-group effect for change in Systemic Symptoms with the score decreasing (worsening) in CON (− 1.1 ± 0.7 /7) while maintaining in EX (0.5 ± 0.5 /7, Fig. 5). A medium-to-large between-group effect was observed for change in Fatigue which worsened slightly in CON (− 0.3 ± 1.2) and changed minimally in EX (0.2 ± 0.8). No meaningful changes were observed in other HRQoL categories (Fig. 5, Table 3).
Change in health-related quality of life from the Chronic Liver Disease Questionnaire (CLDQ). Solid black bars = EX (n = 7), Solid grey bars = CON (n = 4). Error bars represent confidence intervals for change scores. *p value from between-group ANCOVA. Scores from the CLDQ refer to that experienced in the last two weeks. Responses are a Likert scale ranging from 1 (most impairment) to 7 (least impairment). A reduction in the change score represents a lowering of QoL
Other Health Variables
There were no significant between-group effects for change in vascular health outcomes, inflammation, clinical biomarkers including cytokines, habitual physical activity or dietary intake (Table 3; Supplementary Material 3: Results, Supplementary Material 4: Table S3).
Discussion
This study examined the safety, feasibility, and efficacy of HIIT in people with biopsy-confirmed NASH. Consistent with the findings in other chronic disease populations [14], HIIT was safe and feasible in people with NASH, despite high levels of polypharmacy and multimorbidity, including musculoskeletal issues (100%), obesity (92%) and T2DM (75%), in this group. HIIT also elicited meaningful improvements in exercise capacity and improved peripheral insulin resistance, compared with control.
Due to its vigorous nature, the safety of HIIT in clinical populations is often questioned. In the present study there were no adverse events related to HIIT. This is consistent with a large review evaluating the safety of HIIT in stable coronary heart disease (n = 4846), which identified only one non-fatal cardiac event in 23,182 h of HIIT [17]. Collectively, evidence suggests that HIIT, when supervised by an appropriately qualified exercise professional and conducted with adequate screening and monitoring protocols, is safe in clinical populations [14, 16, 17], including NASH.
Despite the presence of condition-specific barriers (e.g., pain and fatigue), 75% of participants who commenced HIIT completed the 12-weeks training. Importantly, all participants who completed the program met the criteria for global adherence to HIIT including attendance, intensity targets and completing the required number of interval bouts. Moreover, the three participants who discontinued HIIT also met these criteria for the sessions they attended. Acceptable levels of session attendance were also recently reported by Stine et al. with 89% of exercising participants with NASH completing > 80% of exercise (5 × 30 min moderate aerobic intensity) sessions [11]. These findings have important ramifications for people with NASH, notably with high levels of comorbid obesity, T2DM and musculoskeletal limitations, for whom higher intensity exercise may typically be viewed as unattainable. Indeed, previous reports have indicated that people with NAFLD have difficulty exercising and performing daily physical activity [20] and as reported by Kistler et al., people who were more likely to report meeting vigorous physical activity targets were younger, had a lower BMI and were not living with diabetes [12]. This study demonstrated that mid-older age individuals with NASH, with a high BMI and comorbid diabetes, can safely adhere to vigorous physical activity, under guidance. This is important as new guidelines for obesity management recommend HIIT as an emerging strategy for the modulation of ectopic adiposity (specifically liver fat) [39], based on the evidence for efficacy of HIIT in people with NAFLD [13]. However, there is a disconnect between evidence-informed recommendations and current clinical care. Healthcare professionals have reported feeling inadequately trained and resourced to effectively target lifestyle behaviour change [40]. This, when combined with trepidation regarding the safety of high-intensity exercise, may impact exercise care and referral.
While we anticipated that HIIT would also improve cardiorespiratory fitness in people with NASH [10, 11] the improvement in exercise capacity but not V̇O2peak is not unexpected in this population, given the different physiological mechanisms for the two measures. Cardiorespiratory fitness reflects the integrated system capacity for oxygen transport, uptake and utilization; while exercise capacity refers to the ability of an individual to undertake a physical task. The observed improvement in exercise capacity is likely due to an improved movement efficiency at submaximal work rates potentially due to increased ventilation efficiency and/or improvements in mitochondrial efficiency [41]. Conversely, exercise-induced improvements in V̇O2peak are largely driven by cardiac remodelling resulting in improved stroke volume via increased in end-diastolic volume [42], which may be blunted in people with long-term chronic disease [43, 44]. Training-induced improvements in exercise capacity and not cardiorespiratory fitness have also been observed in related populations including people with chronic kidney disease [45] and in T2DM [46]. Importantly, data supporting the potent benefit of cardiorespiratory fitness on cardiovascular disease-related and all-cause mortality are predominantly drawn from assessment of exercise capacity (time-on-test, which is then used to estimate V̇O2max) [47, 48]. The ~ 100 s improvement in exercise capacity observed in this study would likely increase capacity to undertake activities of daily living and reduce the risk of cardiovascular disease-related and all-cause mortality.
NASH is associated with both systemic and hepatic insulin resistance [8, 49]. The large effect of HIIT on insulin sensitivity was driven in part by a worsening of peripheral glucose disposal in CON. Nevertheless, there was a 1 mg/KgLegFFM/min improvement in EX and our secondary analysis combining all participants who did HIIT showed a 2.5 mg/KgLegFFM/min within-group improvement. Similarly, Cuthbertson et al. observed a significant improvement in clamp-assessed peripheral and adipose tissue insulin sensitivity following 16-weeks of moderate-intensity aerobic exercise (n = 12) compared with a non-exercise control (n = 7) in people with NAFLD without comorbid T2DM [50]. This improvement was accompanied by reductions in liver fat and increases in cardiorespiratory fitness. Given the size capacity restrictions to DXA imaging, data were normalised for leg FFM rather than total FFM which makes direct comparison with other studies challenging. Without normalisation for FFM, the glucose disposal rates measured in our NASH participants after HIIT training remained about 25% of those observed in healthy aged-matched individuals [8]. Therefore, despite clinically meaningful improvements, severe insulin resistance persisted.
Whilst we observed large between-group effects for change in visceral adiposity and total cholesterol, we did not observe any meaningful between-group effects for markers of inflammation or liver fibrosis. These observations are in line with other exercise studies in NASH [9, 11]. Although not statistically significant, there was a clinically meaningful (> 1 m/sec) reduction in pulse wave velocity, which has been associated with a reduction in risk of cardiovascular events in similar cohorts where arterial stiffness is elevated [51, 52]. Moreover, our study shows promise that exercise may improve (or prevent a decline) in systemic symptoms, which is in line with previous research demonstrating within-group reductions in pain interference and sleep disturbance in response to exercise training in NASH [11].
Findings of this study should be considered within the context of its limitations. Notably, our sample size was small, which is inherent in well-controlled supervised exercise studies in people with NASH; and was further challenged by the COVID-19 pandemic restrictions. This limits the interpretation of some variables such as cytokines and vascular health outcomes. However, while numbers are small, these participants increase the sample of people with NASH who have undertaken an exercise intervention [7,8,9,10,11] in a clinical trial by over 20%. Moreover, the complex nature of participants’ health status meant that some outcomes were unable to be measured. This highlights the challenges of performing well-controlled exercise studies in this cohort. Importantly, future research should also address the ‘real-world’ feasibility of HIIT, which needs to be established as exercise is rarely sustained following supervised intervention in people with NAFLD [10, 53]. Despite randomisation, the HIIT group were more medicated, which is noteworthy as oral-glucose lowering agents [54] and β-blockers [55] may affect cardiorespiratory fitness. However, the predicted impact would be to weaken our ability to see benefit of exercise rather than unfairly bias it. Our overall findings support that exercise training is feasible and beneficial in people with this level of polypharmacy.
Collectively, the findings of this study suggest that supervised HIIT can be a safe, feasible and effective intervention for NASH. These findings support the need to further explore the clinical potential of HIIT, with long-term follow-up, in people with NASH.
Data availability
De-identified data are available on request to Shelley E. Keating (s.keating@uq.edu.au).
Abbreviations
- NASH:
-
Nonalcoholic steatohepatitis
- NAFLD:
-
Nonalcoholic fatty liver disease
- T2DM:
-
Type 2 diabetes mellitus
- HIIT:
-
High-intensity interval training
- CON:
-
Control
- EX:
-
Exercise intervention
- UQ:
-
The University of Queensland
- COVID-19:
-
Coronavirus disease-19
- HRmax:
-
Maximal heart rate
- RPE:
-
Rating of perceived exertion
- SAE:
-
Serious adverse event
- AE:
-
Adverse event
- V̇O2peak:
-
Peak rate of oxygen consumption
- CPET:
-
Cardiopulmonary exercise test
- VT:
-
Ventilatory threshold
- V̇E/V̇CO2 :
-
Minute ventilation/carbon dioxide production
- TGD:
-
Total glucose disposal
- DXA:
-
Dual-energy X-ray absorptiometry
- FFM:
-
Fat-free mass
- SAT:
-
Subcutaneous adipose tissue
- VAT:
-
Visceral adipose tissue
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- GGT:
-
Gamma-glutamyl transferase
- TC:
-
Total cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- TG:
-
Triglycerides
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- BMI:
-
Body mass index
- ANCOVA:
-
Analysis of covariance
- HRQoL:
-
Health-related quality of life
References
Tilg H, Moschen AR, Roden M. NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol. 2017;14:32–42.
Younossi ZM, Golabi P, de Avila L et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol. 2019;71:793–801.
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84.
EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. Journal of Hepatology. 2016;64(6):1388–1402.
Musso G, Gambino R, Cassader M, Pagano G. A meta-analysis of randomized trials for the treatment of nonalcoholic fatty liver disease. Hepatology. 2010;52:79–104.
Baker CJ, Martinez-Huenchullan SF, D’Souza M et al. Effect of exercise on hepatic steatosis: Are benefits seen without dietary intervention? A systematic review and meta-analysis. Journal of Diabetes. 2021;13:63–77.
Eckard C, Cole R, Lockwood J et al. Prospective histopathologic evaluation of lifestyle modification in nonalcoholic fatty liver disease: a randomized trial. Therap Adv Gastroenterol. 2013;6:249–259.
Hickman IJ, Byrne NM, Croci I et al. A pilot randomised study of the metabolic and histological effects of exercise in non-alcoholic steatohepatitis. Journal of Diabetes & Metabolism. 2013;4:1–10.
Houghton D, Thoma C, Hallsworth K et al. Exercise Reduces Liver Lipids and Visceral Adiposity in Patients With Nonalcoholic Steatohepatitis in a Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2017;15:96-102.e103.
O’Gorman P, Naimimohasses S, Monaghan A et al. Improvement in histological endpoints of MAFLD following a 12-week aerobic exercise intervention. Alimentary Pharmacology & Therapeutics. 2020;52:1387–1398.
Stine JG, Schreibman IR, Faust AJ, et al. NASHFit: A randomized controlled trial of an exercise training program to reduce clotting risk in patients with NASH. Hepatology.n/a(n/a).
Kistler KD, Brunt EM, Clark JM, Diehl AM, Sallis JF, Schwimmer JB. Physical activity recommendations, exercise intensity, and histological severity of nonalcoholic fatty liver disease. Am J Gastroenterol. 2011;106(3):460–468; quiz 469.
Sabag A, Barr L, Armour M, et al. The effect of high-intensity interval training versus moderate-intensity continuous training on liver fat: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2021.
Weston KS, Wisløff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. British Journal of Sports Medicine. 2014;48:1227.
Croci I, Coombes JS, Bucher Sandbakk S, et al. Non-alcoholic fatty liver disease: Prevalence and all-cause mortality according to sedentary behaviour and cardiorespiratory fitness. The HUNT Study. Progress in Cardiovascular Diseases. 2019;62(2):127–134.
Levinger I, Shaw CS, Stepto NK et al. What Doesn’t Kill You Makes You Fitter: A Systematic Review of High-Intensity Interval Exercise for Patients with Cardiovascular and Metabolic Diseases. Clin Med Insights Cardiol. 2015;9:53–63.
Rognmo Ø, Moholdt T, Bakken H et al. Cardiovascular risk of high- versus moderate-intensity aerobic exercise in coronary heart disease patients. Circulation. 2012;126:1436–1440.
Doward LC, Balp MM, Twiss J et al. Development of a Patient-Reported Outcome Measure for Non-Alcoholic Steatohepatitis (NASH-CHECK): Results of a Qualitative Study. Patient. 2021;14:533–543.
Glass O, Liu D, Bechard E et al. Perceptions of Exercise and Its Challenges in Patients With Nonalcoholic Fatty Liver Disease: A Survey-Based Study. Hepatol Commun. 2022;6:334–344.
Golabi P, Otgonsuren M, Cable R et al. Non-alcoholic Fatty Liver Disease (NAFLD) is associated with impairment of Health Related Quality of Life (HRQOL). Health Qual Life Outcomes. 2016;14:18.
Stine JG, Soriano C, Schreibman I et al. Breaking Down Barriers to Physical Activity in Patients with Nonalcoholic Fatty Liver Disease. Dig Dis Sci. 2021;66:3604–3611. https://doi.org/10.1007/s10620-020-06673-w
Canada JM, Abbate A, Collen R et al. Relation of Hepatic Fibrosis in Nonalcoholic Fatty Liver Disease to Left Ventricular Diastolic Function and Exercise Tolerance. Am J Cardiol. 2019;123:466–473.
Cortez-Pinto H, Chatham J, Chacko VP, Arnold C, Rashid A, Diehl AM. Alterations in liver ATP homeostasis in human nonalcoholic steatohepatitis: a pilot study. Jama. 1999;282:1659–1664.
Croci I, Byrne NM, Choquette S et al. Whole-body substrate metabolism is associated with disease severity in patients with non-alcoholic fatty liver disease. Gut. 2013;62:1625–1633.
Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381.
American College of Sports Medicine RDEJKLGMM. ACSM's guidelines for exercise testing and prescription. 2018.
Taylor JL, Holland DJ, Keating SE, Bonikowske AR, Coombes JS. Adherence to High-Intensity Interval Training in Cardiac Rehabilitation: A REVIEW AND RECOMMENDATIONS. J Cardiopulm Rehabil Prev. 2021;41:61–77.
Katz LB, Macleod K, Grady M, Cameron H, Pfützner A, Setford S. A comprehensive evaluation of strip performance in multiple blood glucose monitoring systems. Expert Rev Med Devices. 2015;12:263–271.
Keating SE, Hackett DA, Parker HM et al. Effect of aerobic exercise training dose on liver fat and visceral adiposity. J Hepatol. 2015;63:174–182.
Wiley JF, Carrington MJ. A metabolic syndrome severity score: A tool to quantify cardio-metabolic risk factors. Preventive Medicine. 2016;88:189–195.
Younossi ZM, Guyatt G, Kiwi M, Boparai N, King D. Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut. 1999;45:295.
Thijssen DH, Black MA, Pyke KE et al. Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol Heart Circ Physiol. 2011;300:H2-12.
Sehestedt T, H. Olsen M. Chapter 21 - Traditional Versus New Models of Risk Prediction. In: Nilsson PM, Olsen MH, Laurent S, eds. Early Vascular Aging (EVA). Boston: Academic Press; 2015:213–223.
Townsend RR, Wilkinson IB, Schiffrin EL et al. Recommendations for Improving and Standardizing Vascular Research on Arterial Stiffness: A Scientific Statement from the American Heart Association. Hypertension. 2015;66:698–722.
Kavanagh T, Mertens DJ, Hamm LF et al. Prediction of long-term prognosis in 12 169 men referred for cardiac rehabilitation. Circulation. 2002;106:666–671.
Kavanagh T, Mertens DJ, Hamm LF et al. Peak oxygen intake and cardiac mortality in women referred for cardiac rehabilitation. J Am Coll Cardiol. 2003;42:2139–2143.
Kodama S, Saito K, Tanaka S et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. Jama. 2009;301:2024–2035.
Vacha-Haase T, Thompson B. How to Estimate and Interpret Various Effect Sizes. Journal of Counseling Psychology. 2004;51:473–481.
Johnson NA, Sultana RN, Brown WJ, Bauman AE, Gill T. Physical activity in the management of obesity in adults: A position statement from Exercise and Sport Science Australia. J Sci Med Sport. 2021;24:1245–1254.
Hallsworth K, Dombrowski SU, McPherson S, Anstee QM, Avery L. Using the theoretical domains framework to identify barriers and enabling factors to implementation of guidance for the diagnosis and management of nonalcoholic fatty liver disease: a qualitative study. Transl Behav Med. 2020;10:1016–1030.
Broskey NT, Boss A, Fares EJ, et al. Exercise efficiency relates with mitochondrial content and function in older adults. Physiol Rep. 2015;3(6).
Arbab-Zadeh A, Perhonen M, Howden E et al. Cardiac remodeling in response to 1 year of intensive endurance training. Circulation. 2014;130:2152–2161.
Gusso S, Pinto T, Baldi JC et al. Exercise Training Improves but Does Not Normalize Left Ventricular Systolic and Diastolic Function in Adolescents With Type 1 Diabetes. Diabetes Care. 2017;40:1264–1272.
Pandey A, Swift DL, McGuire DK et al. Metabolic Effects of Exercise Training Among Fitness-Nonresponsive Patients With Type 2 Diabetes: The HART-D Study. Diabetes Care. 2015;38:1494–1501.
Beetham KS, Krishnasamy R, Stanton T et al. Effect of a 3-Year Lifestyle Intervention in Patients with Chronic Kidney Disease: A Randomized Clinical Trial. Journal of the American Society of Nephrology. 2022;33:431.
Coombes JS, Keating SE, Mielke GI et al. Personal Activity Intelligence e-Health Program in People with Type 2 Diabetes: A Pilot Randomized Controlled Trial. Med Sci Sports Exerc. 2022;54:18–27.
Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801.
Gulati M, Pandey DK, Arnsdorf MF et al. Exercise Capacity and the Risk of Death in Women. Circulation. 2003;108:1554–1559.
Seppälä-Lindroos A, Vehkavaara S, Häkkinen AM et al. Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J Clin Endocrinol Metab. 2002;87:3023–3028.
Cuthbertson DJ, Shojaee-Moradie F, Sprung VS et al. Dissociation between exercise-induced reduction in liver fat and changes in hepatic and peripheral glucose homoeostasis in obese patients with non-alcoholic fatty liver disease. Clin Sci (Lond). 2016;130:93–104.
The Reference Values for Arterial Stiffness Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values.’ European Heart Journal. 2010;31:2338–2350.
Vlachopoulos C, Aznaouridis K, Stefanadis C. Aortic stiffness for cardiovascular risk prediction: just measure it, just do it! J Am Coll Cardiol. 2014;63:647–649.
Pugh CJ, Sprung VS, Jones H et al. Exercise-induced improvements in liver fat and endothelial function are not sustained 12 months following cessation of exercise supervision in nonalcoholic fatty liver disease. Int J Obes (Lond). 2016;40:1927–1930.
Hamasaki H. Effects of glucose-lowering agents on cardiorespiratory fitness. World J Diabetes. 2018;9:230–238.
Nielen JTH, de Vries F, van der Velde J et al. The Association Between β-Blocker Use and Cardiorespiratory Fitness: The Maastricht Study. J Cardiovasc Pharmacol Ther. 2019;24:37–45.
Acknowledgments
The authors thank Mr Aiman Al Najjar and Mrs. Nicole Atcheson for their magnetic resonance imaging technical support, Ms Marika Carr and Mr Gary Wilson for their biochemistry and laboratory support, Dr Ravin Lal for his technical support conducting cardiopulmonary exercise tests, Mr Todd Gumbleton, Ms Lisa Rich and Ms Lauren Stone for their technical assistance with the euglycemic hyperinsulinaemic clamp, Dr Andrea Fernandez for her medical input, Mr Riley Brown for his assistance with the Metabolic Syndrome Severity Score, Queensland Facility for Advanced Bioinformatics (QFAB, Metro South Hospital and Health Service, Brisbane, Australia) for their statistical support, Professor Danny Green for vascular health software provision, Professor Wendy Brown for mentorship and ongoing scientific discussion, and Ms Kirsten Adlard, Dr Trishan Gajanand, and Ms Chloe Salisbury for research assistance.
Funding
This research was supported by grants from the Diabetes Australia Research Program and Exercise and Sports Science Australia. SEK is supported by the National Health and Medical Research Council (NHMRC) of Australia via an Early Career Fellowship (1122190). The funding sources had no involvement in the study design or research processes.
Author information
Authors and Affiliations
Contributions
Study concept and design: SK, IH, JC, GAM. Acquisition of data: SK, IC, IH. Analysis and interpretation of data: SK, IH, JC, GIM (accelerometry), EC (vascular health). Statistical analysis: SK (with support from Quensland Facility for Advanced Bioinformatics). Drafting of manuscript: SK, IH, EC. Critical revision of the manuscript for important intellectual content: all authors (SK, IC, MW, EC, MT, UP, GIM, JC, GAM, IH). Obtained funding: SK, JC, IH, GAM. Study supervision: SK, IC, IH. Medical supervison: GM, MT, UP.
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
All research was conducted in accordance with both the Declarations of Helsinki and Istanbul. Ethical approval was granted by the Metro South and University of Queensland Human Research Ethics Committees.
Informed consent
Participants provided written informed consent prior to participation in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Keating, S.E., Croci, I., Wallen, M.P. et al. High-Intensity Interval Training is Safe, Feasible and Efficacious in Nonalcoholic Steatohepatitis: A Randomized Controlled Trial. Dig Dis Sci 68, 2123–2139 (2023). https://doi.org/10.1007/s10620-022-07779-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07779-z