Summary
On this page:
Endometriosis
Endometriosis is a disease where tissue similar to the lining of the uterus grows in other parts of the body (Endometriosis Australia 2023). It is an inflammatory condition that can be painful, affect fertility and lead to reduced participation in school, work and social activities.
Symptoms of endometriosis vary between individuals. Some people experience no symptoms, while others experience severe pain, heavy menstrual bleeding, bleeding between periods, abdominal bloating, fatigue, anxiety and depression, among other symptoms (Jean Hailes for Women’s Health 2023).
There is no known cure for endometriosis. Treatments are available to manage the symptoms associated with endometriosis and improve quality of life.
For more information on endometriosis see What is endometriosis?.
How common is endometriosis?
The Australian Longitudinal Study on Women’s Health (ALSWH) is a national study focusing on women’s health. The ALSWH provides information about endometriosis among women in 2 specific cohorts–those born in 1973–78 and those born in 1989–95.
According to the ALSWH, around 1 in 7 (14%) women born in 1973–1978 were estimated to have been diagnosed with endometriosis by age 44–49. Among a younger cohort of women born in 1989–95, 8.8% were estimated to have been diagnosed with endometriosis by age 26–31.
As expected, the cumulative incidence of endometriosis increased with age as women have more time to receive a diagnosis (Figure 1). Of women in the 1989–95 cohort who had turned 31, 9.2% were estimated to have been diagnosed with endometriosis compared with 6.9% of women born in 1973–78 at this age. These differences may reflect increased awareness of endometriosis among the general public and health professionals, leading to increased diagnosis among women born more recently.
See How common is endometriosis? For more information on the incidence and prevalence of endometriosis.
Figure 1: Cumulative incidence of endometriosis, by cohort and age

Hospitalisations
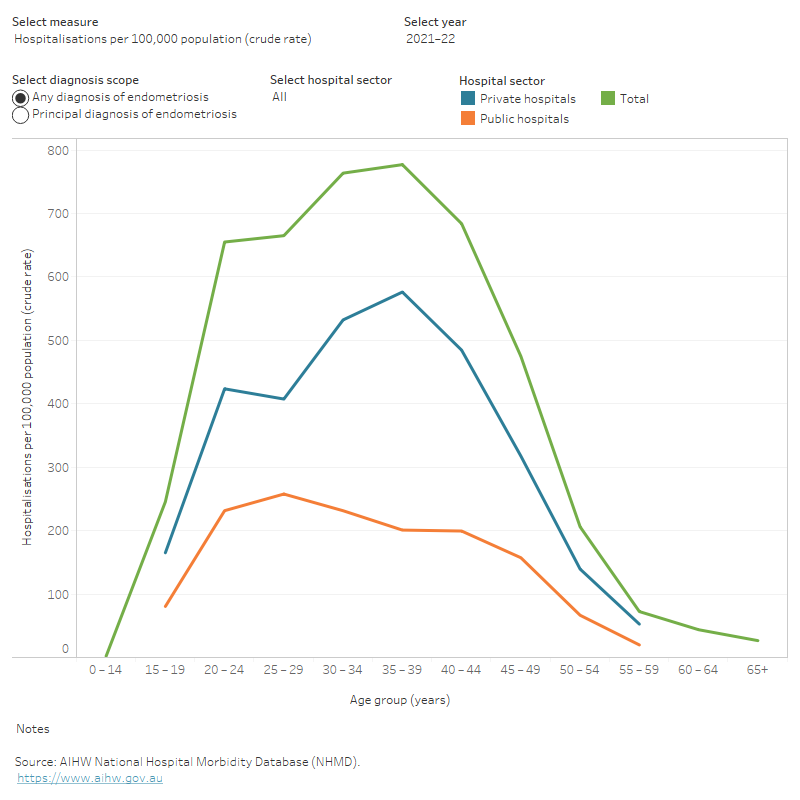
According to the AIHW National Hospital Morbidity Database (NHMD), there were 40,500 endometriosis-related hospitalisations in 2021–22. This represents 312 hospitalisations per 100,000 females. Around half (52%) of endometriosis-related hospitalisations in 2021–22 had endometriosis as the principal diagnosis.
Most endometriosis-related hospitalisations (82% in 2021–22) are among females aged 15–44 (Figure 2), which are generally regarded as a woman’s reproductive years. This represents 18 out of every 1,000 hospitalisations among females in this age group.
The rate of endometriosis hospitalisations has doubled among females aged 20–24 in the past decade, from 330 hospitalisations per 100,000 females in 2011–12 to 660 per 100,000 in 2021–22. This was particularly driven by the increase in the rate of hospitalisations in private hospitals in this period, which more than doubled from 175 to 425 hospitalisations per 100,000 females.
Compared with all female hospitalisations in 2021–22, endometriosis-related hospitalisations were more likely to be partly or fully funded by private health insurance, self-funded, or occur in a private hospital.
See Hospitalisations for more information on endometriosis-related hospitalisations.
Figure 2: Age profile of endometriosis-related hospitalisations, 2011–12 to 2021–22
Alt text: This interactive line chart shows the number, crude rate, and total bed days of endometriosis hospitalisations by age group, hospital sector and year. In 2021–22 the overall number of hospitalisations, rate of hospitalisation and total bed days were highest among females aged 35–39.
Emergency Department presentations
There were more than 3,600 endometriosis-related emergency department (ED) presentations in 2021–22. This represents around 28 presentations per 100,000 females.
Most endometriosis-related ED presentations were among females aged 15–44 (Figure 3). The rate of endometriosis-related ED presentations was highest in the 20–24 age group.
The number and rate of ED presentations due to endometriosis has fluctuated between 2018–19 and 2021–22, peaking at 3,700 presentations in 2020–21.
See Emergency Department presentations for more information on endometriosis-related ED presentations.
Figure 3: Number and rate of endometriosis-related emergency department presentations, by age group, 2021–22

Burden of disease due to endometriosis
Burden of disease is the quantified impact of a disease or injury on a population, using the disability-adjusted life years (DALYs) measure. For endometriosis, there is no burden due to dying prematurely, so only non-fatal burden (YLD) is reported.
In 2023, The Australian Burden of Disease Study found that there were 8,213 YLD from endometriosis in Australia, a rate of 0.61 per 1,000 females (AIHW 2023a). The disease burden due to endometriosis is highest among females aged 30–34 with a rate of 1.71 YLD per 1,000 females.
Endometriosis is the third leading cause of non-fatal disease burden among females due to reproductive and maternal conditions (13%), after genital prolapse (52%) and polycystic ovarian syndrome (26%).
See Burden of disease for more information on the burden of disease due to endometriosis.
Economic burden of endometriosis
According to the Australian Disease Expenditure Study, an estimated $247.2 million was spent on endometriosis in the Australian health system in 2020–21 (AIHW 2023b). The majority (86%) of endometriosis expenditure was attributed to hospitals (including public hospital admitted patient, outpatient and emergency department services and private hospital services).
About 83% of total expenditure on endometriosis was attributed to females aged 15–44 years. Females aged 35–39 years had the highest expenditure amongst all age groups, accounting for around 20% of total endometriosis expenditure.
The cost of disease is not just financial: being unwell has other effects on quality of life, affecting people’s ability to work or do the activities they enjoy. One Australian study estimated the overall cost of endometriosis was $30,900 per person with the condition in 2017, with 84% of this attributed to lost productivity (Armour et al. 2019).
See Economic burden for more information on endometriosis expenditure.
Armour M, Lawson K, Wood A, Smith CA and Abbott J (2019) ‘The cost of illness and economic burden of endometriosis and chronic pelvic pain in Australia: A national online survey’. PLoS One 14(10):e0223316. Doi:10.1371/journal.pone.0223316.
AIHW (2023a) Australian Burden of Disease Study 2023, AIHW website, accessed 14 December 2023.
AIHW (2023b) Disease expenditure in Australia 2020–21, AIHW, Australian Government, accessed 14 December 2023.
Endometriosis Australia (2023) About Endometriosis, Endometriosis Australia website, accessed 1 September 2023.
Jean Hailes for Women’s Health (2023) Endometriosis: Symptoms & causes, Jean Hailes for Women’s Health website, accessed 15 June 2023.


